Fix Primary Care (Part I): A Personal Experience Says It All About Our Failing Health Care "System"
You have a trusted primary care clinician. Your GLP1 medicine works. Now you must spend two hours to jump through more needless hoops to continue treatment. What is wrong with this picture?
—Courtesy (again) of ChatGPT
On June 12, 1987, President Regan stood in Berlin and said, “Mr. Gorbachev, tear down this wall!” The wall came down. The rest is history.
Today, Dr. Len writes, “Mr. Kennedy, fix primary care!” No one will listen, and I doubt many care.
I have shared thoughts these past several weeks about what is broken with health care and how we have lost our focus and lost our way.
Yesterday I had an experience that summarized why we have problems with the health of our nation. Over the next two days I am going to share that experience with you along with a plea that if you do make the effort to read this, my isolated experience will help you understand why so many are losing faith in our health care and why primary care—the most foundational element of good health—is failing.
The chances of fixing this mess are lower than hell freezing over (Adlai Stevenson, “Mr. Ambassador: I am prepared to wait for my answer until hell freezes over.”, United Nations speech about the Cuban missile crisis, October 1962).
That doesn’t mean we shouldn’t focus on the issues, repeatedly, until we get some action.
Let’s begin with the first of two parts (Part II tomorrow):
The Fundamental Principle /Problem
A functioning, organized, effective and personal primary care system is vital to our nation’s health. That ideal no longer exists and is getting worse.
When I was a senior medical officer at the American Cancer Society, my colleagues and I would frequently point out the key to get folks to take care of their health and reduce the risk of many cancers was for an individual to have access to a primary care professional they knew and trusted (and who knew them) as their foremost source of long-term advice and care.
That trusted source of medical care was vital to encourage people to adopt healthy behaviors that reduce the risk of cancer., such as following recommendations for diet, exercise, smoking cessation and cancer screenings. That was the single most effective means of getting someone to follow recommendations proven to improve their health.
As someone who has been a patient, a medical oncologist and a primary care physician, I can tell you when I was critically ill I was fortunate to have a team of people I knew and trusted usher me through my illness. Whether I would live or die—and it wasn’t clear where I was headed--I knew there were folks by my side who gave a damn about me.
We don’t have those relationships anymore.
So many forces have worked to tear down the fundamental relationships we used to have in health care.
How about just a few to start the conversation:
“Managed” care
Large impersonal health care systems aiming for greater efficiencies and income to “feed the beast”
Pharmaceutical companies that no longer find it profitable to manufacture the safe medicines we need to treat our typical chronic diseases (which now cost pennies a day). Instead, we pay exorbitant amounts of money compared to other countries for new medicines that do have miraculous benefits and until recently were only dreams on a shelf
Call centers that put us on hold to schedule or reschedule appointments, that are six months later than we need them
“Step therapy” where insurers say they have your health in mind every January 1 and make you change your successful medications to something more “cost effective
“Provider panels” where the needed specialist is two hours from your home and no longer takes your insurance
If any of this rings your bell then you understand the daily frustration of primary care health professionals who struggle to deliver your care every day or a patient who needs that care when they are ready and willing to get it.
The fundamental takeaway messages?
· Honor primary care.
· Fix the system so clinicians can spend their time caring for patients.
· Improve availability and access to quality, effective care for ordinary people when they need it—and get them in the door easily and consistently so we can do the heavier, long-haul care we need to do.
· Get chronic diseases under control and prevent them in the first place.
What we are doing today won’t cut that mustard. We are failing. Acknowledge the truth and fix the problem.
The Scenario
I have unknowingly been “setting the scene” for this story since I started writing this blog a couple of weeks ago. Go back through my posts and you can pick out the messages. I am not going to review them in detail here, however that is not because they are not relevant. They are very much a part of this discussion.
Now to my reality:
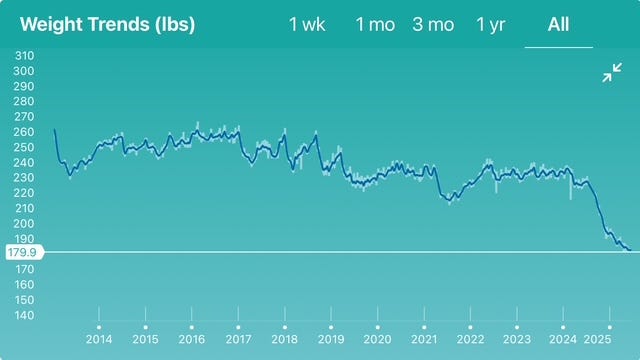
Here is my daily weight chart. It starts at 261.9 pounds in January 2013. The latest entry is 183.3 pounds this morning. It verifies the premise of this story:
My journey:
· I have been overweight or obese my entire life.
· I have suffered with the same chronic anxiety a lot of you do about my weight and its impact on my health.
· My weight has gone up and down over those decades.
· Even though my weight has decreased over the past several years, my BMI was not in a “healthy” range.
· I have metabolic syndrome and all that it entails, I take my medicines to treat my blood pressure, cholesterol and gout every day.
· I have tried and tried and tried to lose weight and keep it off. I have been on countless diet programs since about 2001 through August 2024—and have always relapsed.
· I am fortunate to have a wonderful primary care physician who knows me, knows my medical history, has all my medical information at her fingertips and knows the science. She knows me, my health, and my medical history.
· I was overweight, my BMI met the pre-established threshold to be eligible to have the medication.
· My wife’s employer covered most of the cost through our health insurance.
· I started Zepbound in early August 2024.
· My appetite decreased, the “food noise” went away for the most part, I quickly started to see results.
· I have lost about 50 pounds since August.
· My metabolic syndrome is better, my functional capacity for the most part is good. I am in a much better place than I was before I started the GLP1 medication.
· For the first time since I can remember, I am no longer “husky”, overweight or obese.
· I am incredibly grateful.
The Problem
These new GLP1 medications are expensive. Many employers can’t (or won’t) shoulder the costs. Governments won’t pay for them. And those that do cover them are now withdrawing coverage or putting “lifestyle programs” in the way of quality medical care to “help” patients focus on long term behavior change to lose weight before “approving” payment for the drugs.
Recently, one of the major insurers went a step further and said IF someone has an employer who will pay for the drug, THEN the insurance company will only cover one alternative, in my case the less effective one. I have written about that previously (found here) so won’t repeat the story here. Millions of folks are worried they will have to switch medicines. Their clinicians are worried as well.
No matter: the health plan executives are doing tap dances all over the place around the key questions of efficacy, falling backwards to defend their decision. Screw the patients and the professionals who care for those patients. “We are cost effective and providing quality care.”
Bullshit.
Enter the lifestyle programs.
Once again, I have recently detailed my experience with the demand that I sign up for one of those apps to help me on my weight loss journey if I want my insurance to cover most of the cost of my medication or even cover it at all.
I wrote about that experience recently (found here). I was not happy about the requirement.
Moreover, these programs don’t have valid proof of effectiveness. Apps and programs have come and gone. We are still overweight and obese as a nation, and while a small minority of folks find success long term, the odds are overwhelming that these new apps haven’t discovered something new under the sun. They have just repackaged and fancified the package for the same old stuff that didn’t work before and is not likely to work now. There is no magic to fix this problem. The causes are buried deeply in our brains and our psyches. We are doomed to always find something to express our bad behaviors.
That’s why we now recognize being overweight and obese as diseases, and not choices.
Let me make something clear:
I believe that lifestyle interventions are valuable. People should have options to improve their weight loss journey. Some folks may find “coaches” helpful. Recording daily food intake can work. We could all do better when it comes to exercise.
I believe all of that and more. But having personally worked in the industry of apps, coaches and good intentions, I can tell you that success is difficult to find, even with all the technologies, nudges and analytics now available. You need two partners at the end of those equations, innovators on one end and willing recipients on the other. Having mutual successes is difficult to find these days. People can start out enthusiastically, but enthusiasm only takes most of us so far. Persistence of purpose is difficult to find and more difficult to prove.
We won’t be able to fix the problems of overweight and obesity in this country with apps and coaches until we can fix human behavior. I am not optimistic that these new apps are going to do that effectively or provide us with the long term results we need to improve the health of a nation.
Simple observation:
Ain’t likely to happen, folks.
So why these new programs?
There is only one reason this requirement to join this app program was dropped in my lap to “participate” to continue to receive my medication, even with my proven results and a physician who knows what they are doing them and why I need the medicine:
My employer wants to reduce the program costs by having folks throwing up their hands in frustration give up on the idea of getting the medicine. The employer is one that is committed to evidence-based medicine, and they know the evidence shows those apps and those programs don’t work at large scale to have people achieve a healthy weight and good health long term.
Delay, deny, defer, defeat. Everyone wins—everyone except the person who needs the medication in addition to the health of our nation.
Think: “Road kill.” Our health is now nothing but “collateral damage”.
Period. End of story.
(TO BE CONTINUED TOMORROW)





Why does it take 6 months to get a visit with an internist? There are a myriad of reasons. Two are key in my mind.
In 2019, there were an estimated 44,000 hospitalists in the US. The majority of them are primary care physicians.
Earlier this year there were an estimated 12,000 concierge physicians.
Over 50,000 PCPs that are either not serving the general population or are serving those who can afford to pay for easier access.
The hospitalist movement arose and grew rapidly because PCPs are getting crushed. Hospitalists ease the PCP’s burden, but most PCPs no longer see inpatients, fragmenting our care. Concierge medicine arose as an answer to our PCPs being underpaid and overworked.
There are no easy solutions. In the “best of all worlds” PCPs would have manageable patient loads and schedules that allowed them to provide true primary care.
Unfortunately, that is not the world we live in.